Do you wake up after a full night’s sleep feeling tired and listless? Do you have difficulty falling asleep despite how tired you feel? Or perhaps you can’t seem to stay asleep, tossing and turning throughout the night. If any of these symptoms ring true for you, the chances are good that you’re suffering from insomnia.
Insomnia affects up to one-third of all adults and is one of the most common sleep complaints. Women tend to experience insomnia more frequently than men because of our biological factors such as menstruation, pregnancy and menopause.
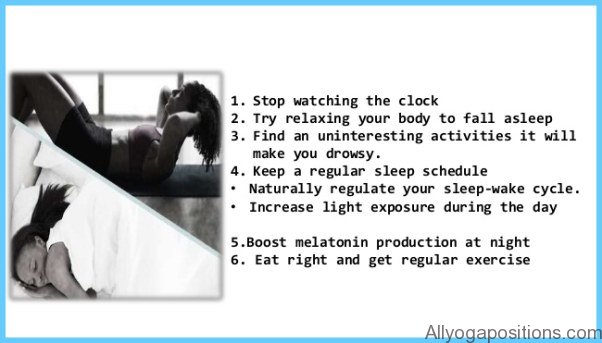
Most of the time insomnia is a symptom of some other health condition. Insomnia has been linked to a variety of medical and emotional disorders. Studies have shown that insomnia can have a devastating effect on everyday life. It can result in decreased productivity, increased motor vehicle and job-related accidents and higher rates of mental and physical illness. There are a variety of ways to treat insomnia, but the best results come from lifestyle management techniques that improve your ability to relax and manage stress.
What Causes Insomnia?
Sleep is a basic human need. When we sleep, our minds and bodies rest and restore energy, preparing us for another day. Most people need between seven and eight hours of restful sleep each night to maintain good health and to feel mentally alert during the day.
Insomnia, the inability to sleep, is a term that refers to a number of different sleep disruptions and disturbances including
• difficulty falling asleep
• waking up early in the morning and being unable to return to sleep
• waking up frequently during the night or having difficulty staying asleep
• waking up after a full night’s sleep and not feeling rested
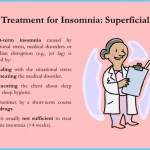
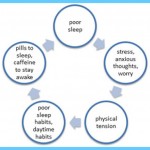
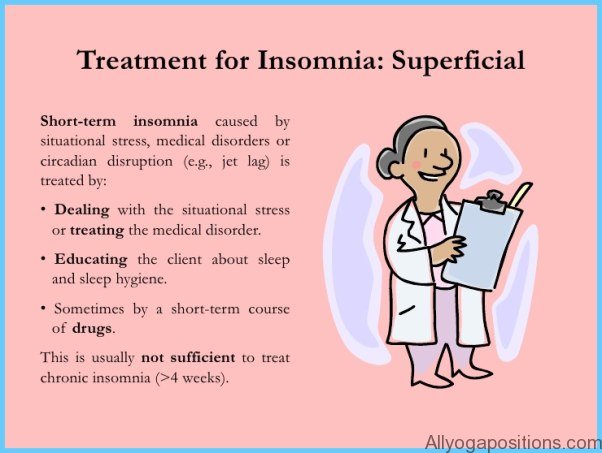
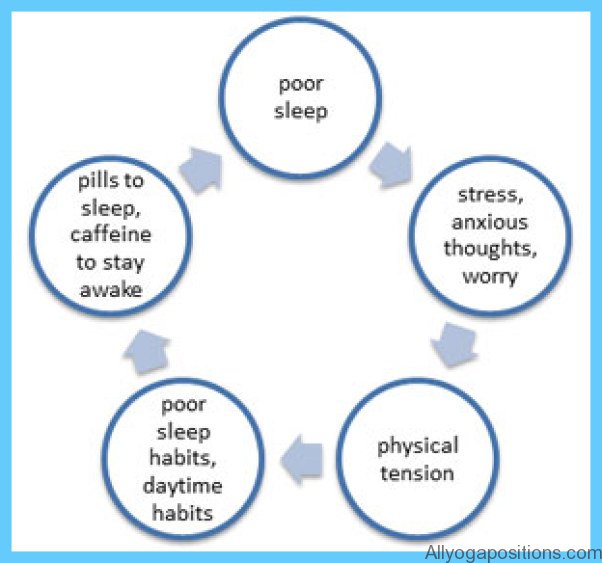
Every once in a while, we all toss and turn through a sleepless night. This is known as short-term or transient insomnia, and is rarely a cause for concern. Only when your sleep habits are disturbed regularly for more than three weeks are you considered to be suffering from chronic insomnia. Insomnia usually results from a combination of factors and is often a symptom of some other physical or mental condition that is affecting you.
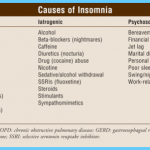
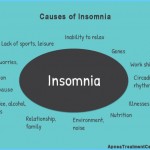
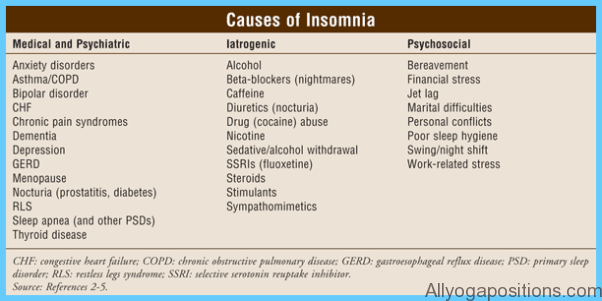
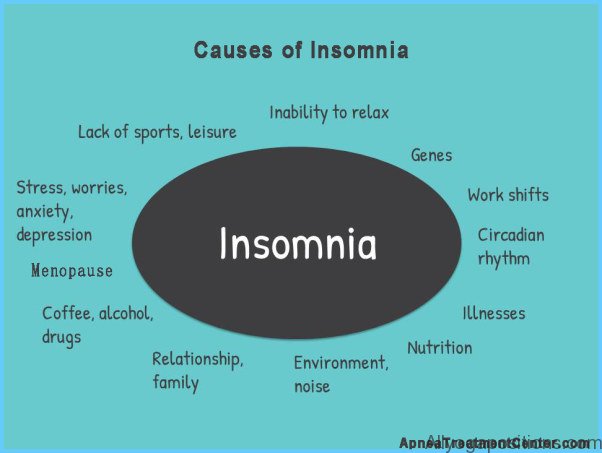
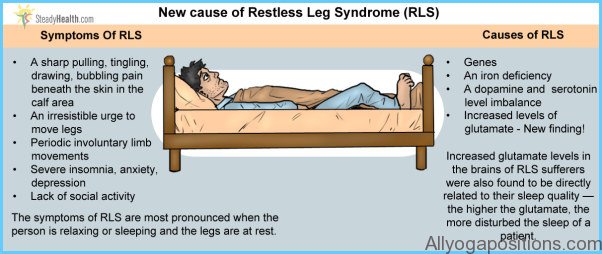
Insomnia is often associated with psychiatric disturbances and is especially common in people with depression and anxiety disorders. Alzheimer’s disease and other forms of dementia can also disturb sleep and cause repeated nighttime awakening. People suffering from arthritis, kidney or thyroid disease, asthma, restless leg syndrome, sleep apnea and gastrointestinal disorders will frequently experience pain and discomfort severe enough to interfere with normal sleep patterns. As well, medications used to treat these and other health conditions may trigger insomnia as an unwanted side effect.
Our sleep patterns change as we age. Research indicates that sleep efficiency decreases from a high of 95 percent in adolescence to less than 80 percent in old age. Consequently, older people have more difficulty falling asleep or staying asleep, and often find that sleep is not as refreshing as it used to be. But there are also many lifestyle and environmental factors that can lead to chronic insomnia. You may suffer from insomnia if you:
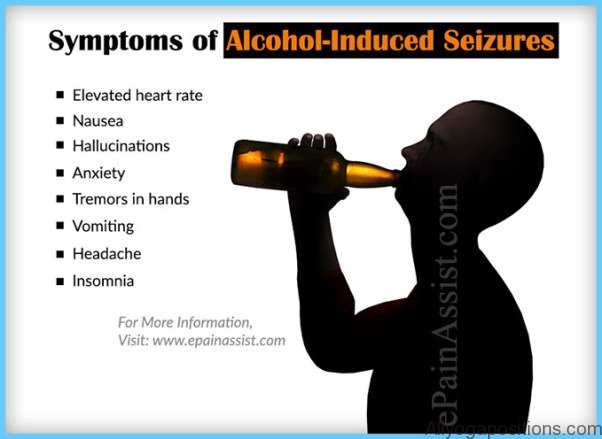
• drink excessive amounts of alcohol or take recreational drugs
• drink coffee or caffeinated beverages before bedtime
• smoke cigarettes before bedtime
• take long naps in the daytime or evening
• disrupt your day/night (or sleep/wake) cycle with shift work or travel that results in jet lag
• experience chronic tension or stress, or worry excessively
• sleep in a noisy environment
• sleep in a room that is too warm or too cold
These factors are often responsible for the development of sleep problems and they may also prolong the symptoms of existing insomnia. Simple adjustments in sleep habits and lifestyle can go a long way towards helping you get a good night’s sleep.
Insomnia is much more common in women than it is in men. In general, women tend to sleep fewer hours and to experience a poorer quality of sleep, especially as they get older. Fluctuating hormone levels are the primary culprits. As the levels of estrogen and progesterone hormones change in response to menstrual cycles, pregnancy and menopause, women are more likely to suffer ongoing sleep disturbances that rob them of energy, health and mental agility.
1. Menstruation Poor quality sleep is often associated with the beginning of the menstrual cycle, when bleeding starts. Some women feel particularly sleepy and fatigued when progesterone levels rise right after ovulation. As the menstrual cycle continues, progesterone levels begin to fall rapidly, signaling the start of menstruation. This is a time when many women are quite wakeful and find it difficult to fall asleep at night.
2. Premenstrual Syndrome (PMS) During the latter part of the menstrual cycle, some women struggle with the debilitating symptoms of PMS. In addition to bloating, moodiness, abdominal cramps and irritability, women with PMS may find it hard to get to sleep or to stay asleep or they may sleep excessively. Insomnia and the associated daytime tiredness are common symptoms of PMS.
3. Pregnancy The physical and emotional demands of pregnancy often lead women to report more disturbed sleep. Rising levels of progesterone in the first trimester are known to increase sleepiness. In the early stages of pregnancy, sleep patterns may also be disrupted by the need to urinate frequently. In the second trimester sleep quality tends to improve but is still worse than before pregnancy. Most pregnancy-related sleep problems develop during the third trimester, when the fetus puts pressure on the bladder, increasing the need to go to the bathroom during the night. Heartburn, sinus congestion and leg cramps are also common in the later stages of pregnancy and will cause enough physical discomfort to disturb sleep. Once the baby is born, a mother’s sleep is interrupted often, and the resulting sleep deprivation may trigger emotional problems such as a mild depression known as post-partum blues.
4. Menopause As a woman ages, her levels of estrogen and progesterone begin to drop, and eventually she stops menstruating. This transition to actual menopause (cessation of menstruation) is the time when women report the highest levels of sleep disruptions. In many cases, insomnia is brought on by night sweats, which are hot flashes that occur during sleep. Women in menopause often experience daytime tiredness and chronic fatigue.
Who’s at Risk?
According to the National Sleep Foundation, nearly two-thirds of Americans experience sleep problems. Although people of all ages can experience insomnia, it seems that women experience it more frequently than men and are more willing to seek treatment. Insomnia is also common among the elderly. Studies have indicated that people coping with stressful situations, such as divorce or unemployment, or who have medical or emotional conditions, are much more prone to insomnia. Those who have sleep disturbances that persist for more than 12 months are also more likely to develop depression, anxiety disorders and alcohol dependency.
Diagnosis
Insomnia can be difficult to diagnose. The need for sleep varies from individual to individual. Some people require much less sleep to function effectively than others. This makes it challenging to develop sleep standards and norms for effective diagnosis. Generally, you will be diagnosed with insomnia if your sleep disturbances are severe enough to noticeably affect your daytime mood and activities. Determining the frequency, intensity and duration of your sleep disruptions is also helpful in making an accurate diagnosis.
Because insomnia is so often a symptom of another disorder, the American Medical Association recommends that the real emotional, physical or environmental causes of insomnia be diagnosed and treated, before any other steps are taken to treat insomnia complaints. To do this, your doctor will evaluate your sleep patterns, your drug use (including alcohol, nicotine and caffeine), your psychological and physical condition and your level of physical activity. In some cases, you may be sent to a sleep laboratory for further testing.