Simply being in pain is stressful, for your brain interprets it as a threat and activates the body’s stress mechanisms. When this situation persists, elevated levels of stress hormones such as cortisol tax your body’s resiliency, causing burnout and inhibiting recovery mechanisms. Prolonged cortisol surges triggered by continual stress also inhibit the creation of new nervous system tissue, slow down learning and memory, and help perpetuate existing emotional distress.
It doesn’t matter if the stress and pain develop simultaneously or the stress ensues later: Unremitting stress makes it difficult for the nervous system to calm down. That’s why the stressed-out “pain brain” is always on edge, hyper-aroused, and feeling everything more intensely, including pain sensations. It’s as if the pain volume has been turned up; there’s more of it and it hurts more. This phenomenon is called central sensitization, and when it strikes, it takes less provocation to trigger more pain. Your body can hurt in response to simple things like being touched or changes in the weather.
Trauma and the Pain Experience
Trauma is a serious and often over-looked problem among chronic pain patients. Whether mild, moderate, or severe enough to qualify as PTSD, signs of trauma are exhibited by up to half of all chronic pain patients—tens of millions of people.
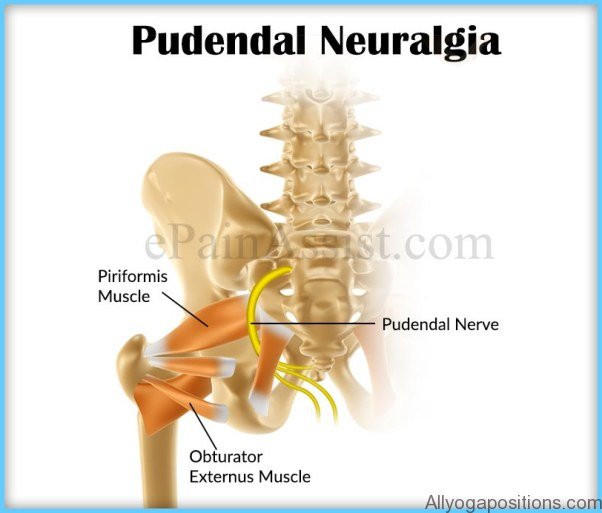
Yoga Poses For Chronic Pelvic Pain Turn Up the Pain Volume Photo Gallery
When pain doctors and psychologists talk about trauma, they’re referring to a patient’s emotional response to an accident, sexual assault, natural disaster, or any other terrible event or period of time. Whether or not she was physically harmed during the traumatic event, the patient develops an intense emotional reaction that may include mood swings, flashbacks, nightmares, social isolation, and other problems.
As I write this, I am treating a patient named Aaron who is suffering from severe pain in his lower back. He’s an enthusiastic gym-goer who loves to throw himself into weight lifting and basketball, and rides a bicycle on his non-gym days. We don’t know how it happened, for there was no specific fall or injury, but he recently wound up with a herniated L5-S1 disc that is causing him tremendous pain. It’s gotten to the point where he can barely sit and cannot sleep through the night. His brain, interpreting this pain as a life-threatening situation, has triggered the fight-or-flight response. And this has sent his blood pressure to sky-high levels over the past week. But he’s not suffering from mood swings or other trauma symptoms because he hasn’t had an intensely negative emotional reaction to whatever it was that caused his disc to herniate. In short, he’s avoided the trauma experience.
However, I have a second patient, Greg, similar to Aaron in age and other respects, who suffered exactly the same L5-S1 herniation when he was mugged by two big, scary-looking thugs in a dark alley. These two patients have the exact same physical problem, but Greg quickly began exhibiting signs of severe emotional distress. Immediately after the mugging, he went into shock and denial. Soon, Greg was experiencing flashbacks of that terrible event, and exhibited sudden flares of anger and other symptoms of trauma. His back pain has persisted for months, triggering the same continual fight-or-flight reaction experienced by Aaron. But Greg also suffered from trauma, which further aroused his nervous system and made his chronic pain experience worse.
Unfortunately, Greg’s trauma didn’t fade as time passed and his emotional upset persisted until it became full-blown PTSD. This really turned up the dial on his pain. With his brain and body continually awash in stress hormones, Greg’s adaptive pathways began to shut down. His SNS and PNS could not work in concert to rev things up then cool things off as necessary. Instead, Greg was in a constant state of agitation, adding another dimension to fight-or-flight known as “freeze.” Freeze is a state in which a patient is so overwhelmed that it becomes difficult to handle even basic daily tasks. Once a person becomes frozen by their trauma, healing cannot occur until healthy brain processing has been restored.
Trauma Reactivation
Sometimes the memory of past traumas stored or hidden inside the brain can be “reawakened.” A new experience of pain, an injury, or some other stressful event can “wake up” old trauma messengers, even though the trauma may have occurred years earlier and is completely unrelated to the present pain problem When this “trauma reactivation” occurs, the person in pain does not actually recall the past traumatic event. But he relives the intense emotional response that it created.
Knowledge of a person’s life experiences, and piecing together how these experiences may be affecting him today, is an important part of understanding that person’s pain. At my center, we perform a comprehensive assessment that includes an in-depth psychological evaluation that looks at past traumas. These traumas come from many sources, including physical, emotional, or sexual abuse, and while it doesn’t necessarily cause a back injury or a car accident later in life, it can significantly impact how a person responds to these events by overstimulating the brain’s response to pain, and prompting the fight-or-flight and/or freeze responses. Thus, for many pain patients, trauma therapy is a necessary part of the recovery program