Does your life feel out of control for one week out of every month? Does your mood swing from depression to anger at the drop of a hat? Do you feel emotional, tearful and anxious? Do your insatiable cravings for junk food only aggravate the suddenly too-tight fit of your clothes? If you answered yes to one or more of these questions, then you’re only too aware that these are symptoms of premenstrual syndrome (PMS). If you suffer from PMS, you’re not alone. Countless women all over the world struggle to cope with symptoms like these each day. It’s estimated that PMS affects 30 to 40 percent of all women during their childbearing years.
Your Monthly Cycle
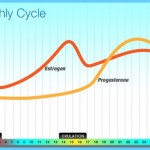
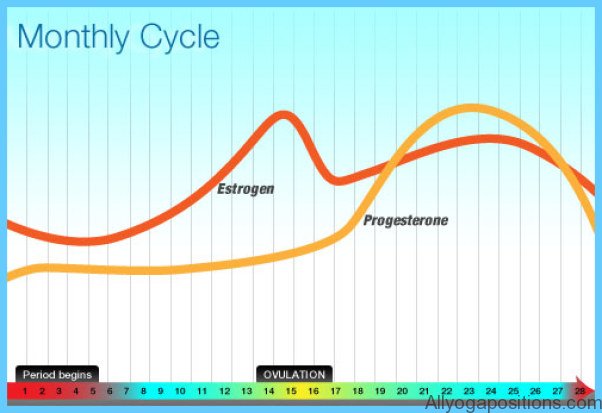
Counting the first day of your period as the beginning of your four-week menstrual cycle, the symptoms of PMS appear during the last two weeks. These two weeks are referred to as the luteal phase of your cycle. In fact, there are three distinct phases in each menstrual cycle: the follicular phase, ovulation and the luteal phase. Two areas of the brain, the hypothalamus and the pituitary gland, control all the hormonal changes that regulate each of these distinct stages.
The menstrual cycle begins with the follicular phase of your cycle, which lasts from the first day of your period until the time you ovulate. It begins when the hypothalamus produces gonadotropin-releasing hormones (GnRH). These hormones pass into the pituitary gland and trigger the release of luteinizing hormone (LH) and follicle-stimulating hormone (FSH). Working in combination, these two hormones promote the growth of follicles, tiny saclike structures located in your ovaries, each one surrounding an ovum, or egg. Throughout this time of growth, the follicles produce most of the female sex hormone, estrogen, which circulates in your body. Between 10 and 20 follicles will enlarge, but normally only one egg is released during ovulation.
Ovulation occurs in the middle of your cycle, near day 14. It’s at this time that hormone surges trigger one follicle to burst and release its egg. Over the next 36 hours, the egg will travel through your fallopian tubes to reach the uterus.
After ovulation, your body enters the luteal phase. The outer wall of the burst follicle remains in your ovary and transforms into a mass of tissue called the corpus luteum. This tissue begins to secrete the other female sex hormone, progesterone, which prepares your uterus for pregnancy. If the egg is not fertilized and pregnancy doesn’t occur, the levels of estrogen and progesterone immediately begin to drop. The lining of the uterus and the unfertilized egg are no longer needed and are eliminated from the body through menstruation. This completes the menstrual cycle and the entire process starts all over again.
What Causes PMS?
Researchers don’t know exactly what triggers PMS, but several theories are under investigation. One of the most popular theories suggests that PMS is caused by an imbalance in the levels of estrogen and progesterone. Symptoms may develop because women have too much estrogen and not enough progesterone in their system during the last two weeks of the menstrual cycle. Estrogen affects the kidneys and causes sodium and water retention. Alterations in estrogen and progesterone can also affect the levels of natural brain chemicals called neurotransmitters. It’s thought that deficiencies in serotonin and dopamine, two neurotransmitters that affect mood and emotion, may be responsible for the mood swings typical of PMS.
Low levels of progesterone may cause PMS in another way. When progesterone levels drop, so do levels of a related hormone called allopregnanolone. Studies have shown that a deficiency of this hormone may cause anxiety or depression. That’s because allopregnanolone appears to influence a neurotransmitter called GABA (gamma-aminobutyric acid), which plays an important role in anxiety.
Excessive levels of a hormone called prolactin may be responsible for breast tenderness and swelling. Prolactin is responsible for stimulating the breast changes and milk production necessary for breastfeeding.
Nutrient deficiencies may also account for certain symptoms of PMS. For instance, breast tenderness may also be caused by a diet lacking in essential fats, which help regulate pain and inflammation. Recent studies have revealed that a deficiency of calcium can cause many PMS symptoms, including agitation, irritability and depression, by stimulating an overproduction of parathyroid hormones. These hormones are believed to influence mood and mental function by interacting with the brain chemical serotonin. PMS may also be related to dietary deficiencies of vitamin B6, magnesium and zinc, or the condition may be triggered by excessive consumption of caffeine, salt, alcohol and red meat.
Finally, it’s possible that PMS is associated with medical conditions that have a nutritional component, such as hypoglycemia (low blood sugar) or hypothyroidism (low thyroid hormone level).
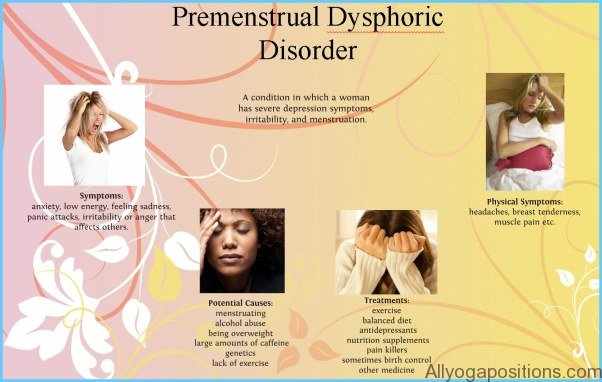
Symptoms
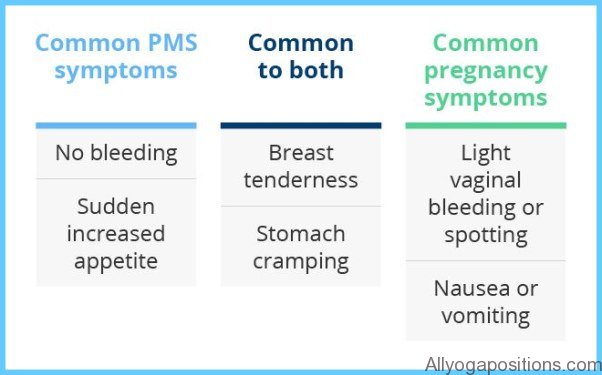
PMS is a collection of emotional, psychological and physical symptoms that develop during the 7 to 14 days before the start of your menstrual period. There are more than 150 documented symptoms with the most common being depression. PMS symptoms tend to fall into two main categories:
1. Physical symptoms include breast tenderness and swelling, bloating, fluid retention, weight gain, headaches, food cravings (especially for sweet or salty foods), acne, muscle pain, backaches, fatigue, dizziness, sleep disturbances, constipation or diarrhea. Many of these physical symptoms are caused by fluid retention, especially weight gain. In my private practice, women gain an average of 2 to 4
pounds during the premenstrual week. Heavier women may gain as much as 8 pounds. Fluid retention can also cause abdominal bloating. And if you experience constipation it will only add to the misery of bloating and weight gain.
2. Emotional or psychological symptoms include mood swings, depression, irritability, aggressiveness or hostility, anxiety, crying spells, changes in sex drive, difficulty concentrating and feelings of low self-esteem.
PMS symptoms vary from woman to woman and they can also be different from one menstrual cycle to the next. In PMS, symptoms get worse as your menstrual cycle progresses and are then relieved when your period begins. When you reach menopause, PMS normally disappears, although the symptoms may recur if you take hormone replacement therapy during your postmenopausal years.
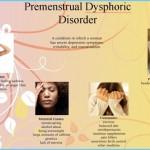
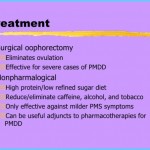
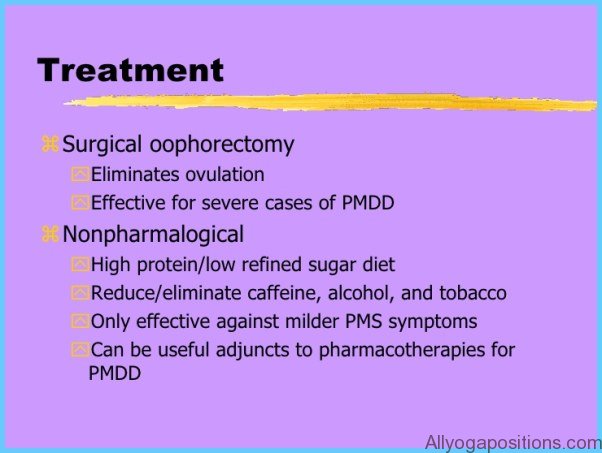
For some women, the physical and emotional changes caused by PMS are so severe that they interfere with their ability to function at work or interact with family and friends. When PMS symptoms seriously undermine quality of life, the condition is called premenstrual dysphoric disorder (PMDD)—a complex medical disorder that has only recently been identified. Thankfully, PMDD affects only a small percentage of women. It’s thought to be an excessive reaction to the normal hormonal changes associated with the menstrual cycle.
Who’s at Risk?
Most women suffer from some type of premenstrual discomfort. In fact, 75 to 95 percent of all women experience one or more of the symptoms that are associated with PMS. But research indicates that only 30 to 40 percent of women between the ages of 25 and 50 years report the recurring symptoms indicative of PMS.1 And only 5 to 10 percent of women develop symptoms severe enough to disrupt lifestyle and daily functioning.
PMS can begin any time after puberty. It’s often triggered by a hormonal shock to your system, usually caused by an obstetrical or gynecological event such as pregnancy, tubal ligation or the use of oral contraceptives. Even women who have had hysterectomies can suffer from PMS if their ovaries are left intact after the surgery. Research suggests that you’re more susceptible to PMS if you’re under a lot of stress,
you’re under 34 years of age or you drink alcohol. Heredity may also play a role; however, PMS symptoms are not consistent in families and vary considerably among female relatives.
Diagnosis
It can be difficult to diagnose PMS because the symptoms mimic those of many other disorders. Before your doctor can diagnose PMS, he or she must first eliminate the presence of another medical condition such as clinical depression, hypothyroidism, chronic fatigue syndrome, diabetes or irritable bowel syndrome.
The classic indicator of PMS is the timing of your symptoms. Your doctor will try to determine if your symptoms occur consistently around ovulation and continue until the beginning of your period. For the diagnosis of PMS to be correct, there must be a symptom-free interval between menstruation and the next ovulation near day 14 of your cycle. If your symptoms persist during all phases of your menstrual cycle, then you may be suffering from some other medical disorder. To help your doctor with the diagnosis, you may be asked to keep a menstrual diary, where you record your physical and emotional symptoms every day for several months. Because there are no laboratory tests that identify PMS, this diary is one of the most important tools used to assess your condition. To make the diagnosis of PMS, your doctor will look for a pattern of symptoms that occur regularly and have a negative impact on your ability to manage personal relationships and function normally at home and at work.
Your doctor will also review your medical and psychiatric history and conduct a thorough physical examination, including a pelvic exam. In some cases, laboratory tests may be needed to rule out other medical conditions.