The Abaci Plan: Restoration, Recovery, and Relief
The Abaci Plan is built around individual approaches or “pieces,” which, taken together, can literally reshape your brain and the way it communicates with your body. By working through the plan, you’ll be able to feel better, become more active, enjoy more satisfying relationships, and reach many of your most cherished goals.
Let’s take a brief look at my core approaches, each of which will be explained in detail in the chapters to follow.
1. Finding calm in the storm—When chronic pain strikes, your nervous system becomes hypersensitive. It’s constantly in the “fight or flight” mode, quick to flood your body with powerful hormones and chemical transmitters that can trigger burnout, anxiety, and other problems. This hypersensitive state, called “central sensitization,” revs up your body’s pain system, overwhelms you emotionally and physically, and makes it nearly impossible for you to think clearly. It’s as if the sensation of pain has been turned way up, like the volume of a radio. Because central sensitization is so overwhelming, the first step in managing chronic pain is calming the nervous system or turning down the “trauma alarm”
You may be surprised to learn that chronic pain and posttraumatic stress disorder (PTSD) are intimately linked. Although one syndrome does not necessarily cause the other, up to half of all people suffering from chronic pain also have symptoms of trauma. In some patients, the trauma and pain begin together, as in a soldier who is seriously wounded in battle. In other patients, an injury may “awaken” a trauma from the past—we often see patients with histories of childhood traumas, whether physical, emotional, or sexual. Although the past and present traumas are unrelated, they begin “feeding” off each other. The new pain recreates the reaction of a distant trauma within the nervous system, which increases the overall sensitivity to pain. In still other patients, the experience of chronic pain itself may become the trauma.
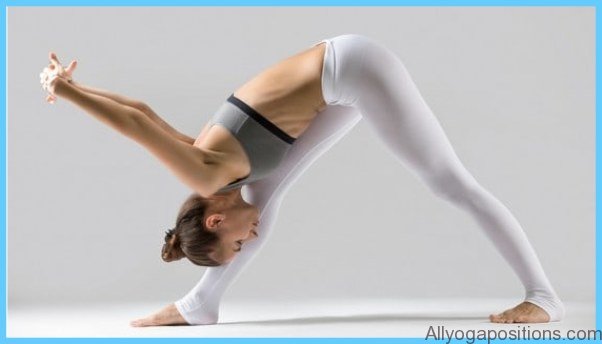
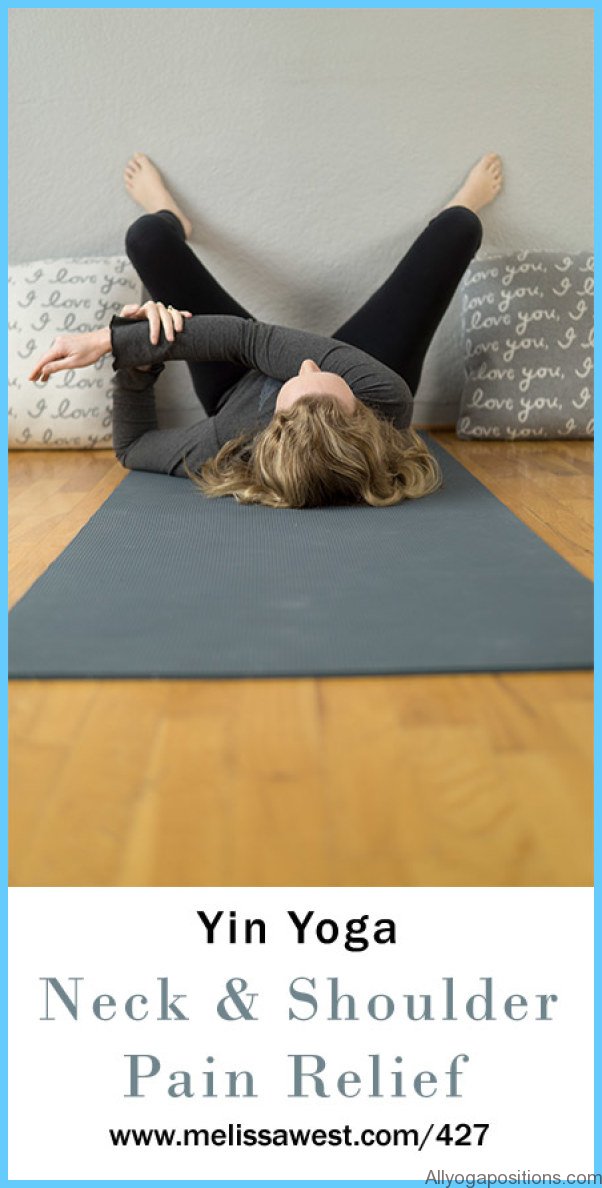
Yoga Poses For Shoulder Pain Photo Gallery
In Chapter 4, you’ll learn about the scientific link between trauma and chronic pain. And you’ll discover effective ways of addressing trauma and the resulting hyper-arousal of the nervous system through mindfulness, meditation, yoga, breathing exercises, and EMDR (eye movement desensitization and reprocessing).
2. Reframing harmful thoughts—Thoughts are not just ideas or notions; they are also part of a process that continually re-forms the brain. What you think really matters, and it can either increase or decrease your pain. Learning how to set aside catastrophic thinking, anger, fear, and other forms of negative thinking can lessen your experience of pain. And replacing harmful thoughts with positive ones can actually heal your brain and help you regain control of your life.
You’ll learn about the connection between thoughts, emotions, and pain, as well as how to reframe your thoughts to avoid the traps that perpetuate your pain. And you’ll discover how to think about your pain, fear, and anger in helpful ways, shifting your focus toward gratitude, love, compassion, and kindness.
You’ll also learn how to accept pain as a path toward relief. Raging against your pain and what it has done to you is a natural reaction that may even feel good. But when you refuse to accept your pain, you can become drawn into unnecessary treatments that create false hopes and put you at risk of serious complications. The best way to control pain is to accept the changes in your life, let go of negative feelings, grieve for your losses if necessary, and then move ahead. Developing realistic expectations about traditional medical treatments can also bring you closer to acceptance.
The path to relief begins with accepting the challenges before you, embracing yourself and all that is good in your life, and activating the healing power within you.
3. Igniting creativity—The “pain brain” is awash in harmful emotions that drive physical pain. These emotions (fear, anger, frustration, and so on) are often deep-seated and difficult for pain patients to address or even describe. In many cases, they don’t even know they exist! Yet these harmful emotions are harbored by almost every pain patient, and act like hidden bacterial infections quietly spewing out poison.
New research shows that art and music can function as medicine, bringing these hidden emotions to the surface, neutralizing many of them, and helping to heal the brain. Using simple techniques, you can use art to unlock your hidden emotions and reshape your brain. It doesn’t matter whether or not you have talent in these areas. Even if you think you can’t draw or sing, art can be a powerful recovery tool.
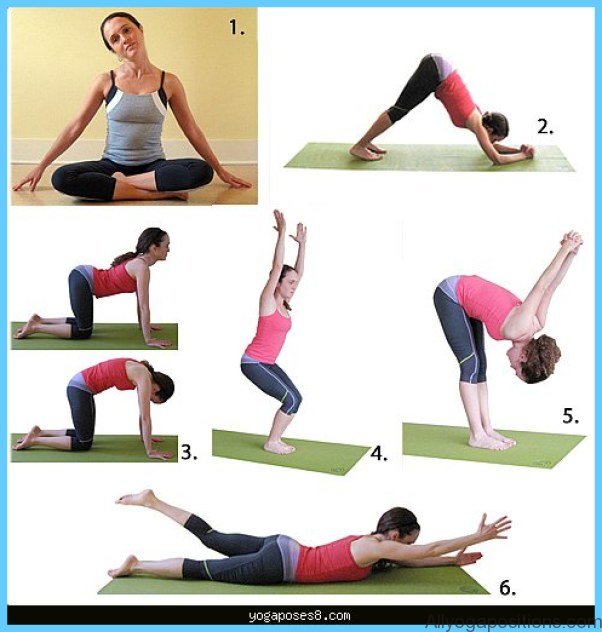
4. Using the medicine of movement—Chronic pain restricts a person’s ability to move, no matter where the pain may manifest. Yet the body functions and feels better when it’s active, which is why movement is a crucial part of the program Indeed, not moving can become a source of pain. The Spanish Inquisition prevented prisoners from moving as a form of torture.
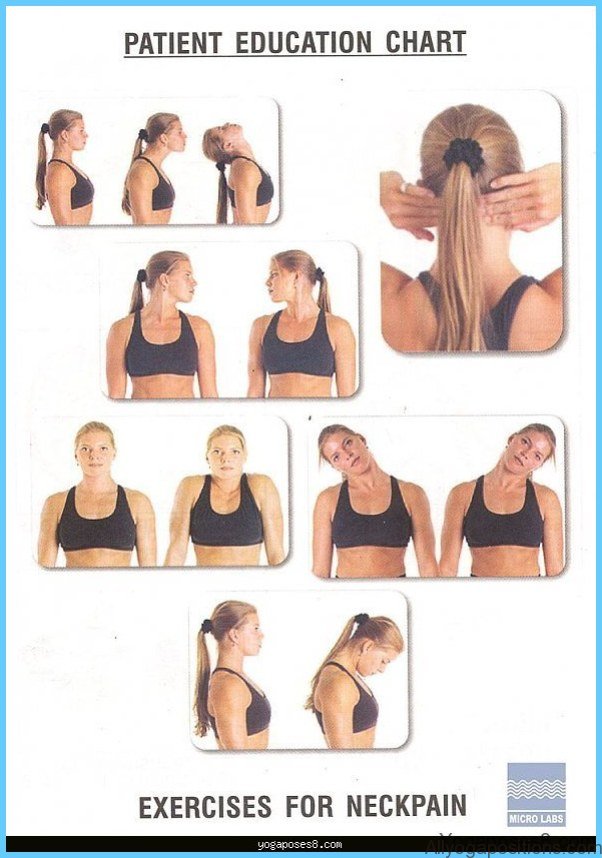
Because even simple activities like walking and stretching can help heal the “pain brain,” in Chapter 7 we’ll look at numerous ways to create movement in your life, no matter what your pain level may be. I’ll present exercises that can maintain and improve your ability to handle daily activities and even get you up and climbing stairs, if possible. To help you go beyond, we’ll examine traditional exercises that strengthen your core and improve your posture, as well as alternative modalities such as yoga, Pilates, tai chi, and chi gong.
5. Ingesting quality—Eating right is important, for certain foods can contribute to inflammation. Excess weight exacerbates certain types of pain, and weight gain is a common problem in those who have been injured, further complicating their recovery. In Chapter 8, you’ll learn how to use food to reduce your body weight and inflammation levels and give your body the tools it needs to heal. Not only will good nutrition help repair the “pain brain,” it can increase your ability to be more physically active, an important part of the healing process.
Because everything you ingest is important, we’ll also discuss reducing or even eliminating your opioid medications, for they often cease to be a solution and become a large part of the ongoing problem
6. Re-charging—One of the most common and aggravating side effects of chronic pain is the inability to sleep. Many of my patients tell me they are tired “all the time,” that they turned to sleeping pills hoping for relief and soon found themselves dependent on pills that really didn’t help. But now they’re too frightened to stop taking them!
In Chapter 9 we’ll explore the links between sleep and pain, stress, medications, food, and other things that interfere with the good night’s rest that pain patients so desperately need. We’ll also talk about techniques that can help you sleep longer and better, even as you turn away from potentially dangerous sleeping pills.
7. Gaining treatment perspective—The American health system is confusing, costly, riddled with contradictory advice, and designed to rush most patients through exam rooms, procedure rooms, and hospitals, and out the door. The faster you move through the system, the faster the money is earned, but that doesn’t necessarily spell success for you. It’s critical that you understand what you can expect, realistically, from our healthcare system
Consider the concept of ROI, or “return on investment.” Because many chronic pain treatments are not covered by standard insurance, they must be paid for out-of-pocket. Given the sometimes high cost of alternative treatments, you’ll need to decide, in advance, if it’s worth the expense. But how do you assess the value of a treatment? How do you put a value on improved quality of life, or balance the extra money spent on one treatment with reduced amounts spent on another? In Chapter 10, we’ll look at ways to answer these key questions.
It’s also important that you understand how physicians view their patients and present their treatment plans, so you’ll know how to use them and their advice to your best advantage. And it’s vital to understand how to evaluate health studies and to research treatment possibilities on the Internet.
8. Mastering time—Time is a major issue in the life of a pain patient. It can function as a negative factor, with the body atrophying rapidly over time, and the brain becoming more and more of a “pain brain.” But time can also be, and should be, a positive factor, with every moment being another opportunity to heal.